Diabetes Prevention, Diagnosis, and Management
By Kristy Warren
November marks Diabetes Awareness Month, which aims to bring awareness to and promote a better understanding of this chronic condition. More than 100 million Americans have diabetes or elevated blood sugar that puts them at risk of developing diabetes (a condition known as pre-diabetes).
Because early symptoms of elevated blood sugar aren't always noticeable, many people don't even realize they have pre-diabetes. So how do you know when to talk to your doctor and how can you prevent elevated blood sugar from developing into diabetes? Our Laurel Health Center experts have you covered with tips for recognizing, preventing, and managing diabetes.
What Exactly is Diabetes?
Glucose is the primary sugar that our body uses for energy, and our pancreas produces insulin. Insulin works like a delivery truck as it shuttles glucose from your bloodstream to your cells to use and store for energy. Diabetes is a metabolic disease that inhibits our body’s ability to properly store glucose in the blood.
In someone with diabetes, the body either does not produce enough insulin or does not use insulin effectively enough. When you don't have enough insulin or your cells are resistant to insulin, glucose builds up in your bloodstream instead of being stored in your cells and leads to elevated levels of glucose in the blood. An elevated blood sugar level can lead to health problems with the heart, kidneys, vision, and circulation.
Pre-diabetes refers to blood sugar levels that are higher than normal but not yet diabetic, putting someone at increased risk for developing type 2 diabetes and other health problems like increasing your risks for heart disease and stroke. More than 80% of those with pre-diabetes do not realize they have the condition.
Where Glucose Comes In
Glucose is the primary sugar that our body uses for energy. When we eat or drink, most of the sugars we consume get broken down into glucose by our bodies and then sent into our bloodstream. The pancreas then releases insulin, a hormone that helps move glucose from our blood into our cells to be used or stored for energy. If you have diabetes, your body isn’t able to move or store glucose well.
Our modern diet contains a lot of opportunities to make glucose, and it is easy to consume too much. A food doesn't need to taste sweet to pack a glucose punch. Starch (a carbohydrate found in bread) and lactose (a carbohydrate found in milk) are both broken down into glucose inside your body. The sucrose, fructose, and corn syrup commonly used in processed foods are also broken down into—you guessed it—glucose. All that extra glucose in our blood must either be used by our organs or packed away into fat or muscle tissue as storage.
Since so many foods and drinks have carbohydrates that break down into glucose, how we store extra glucose is very important. A 200 lb person without diabetes stores approximately 6 grams of glucose in their blood at any given time. For perspective, one can of Coke has 39 grams of carbohydrates, which includes glucose, sucrose, fructose, and corn syrup.

Types of Diabetes
There are different types of diabetes mellitus. While all types of diabetes mean there is too much glucose in the blood, they have different causes and modes of treatment. The "big three" you will hear discussed most often are Type 1, Type 2, and gestational diabetes:
- Type 1 diabetes is when the body stops producing insulin entirely. You may have heard it called “juvenile onset” or “insulin-dependent” diabetes because it is typically diagnosed in someone’s youth and requires daily insulin injections or an insulin pump.
- Type 2 diabetes is when the body doesn’t use insulin properly and/or no longer produces enough insulin. It is the most common type of diabetes and can develop at any age. Type 2 diabetes accounts for over 90% of cases.
- Gestational diabetes affects a mother’s ability to create and use insulin during pregnancy; it occurs in approx. 10% of pregnancies.
Why is Diabetes Dangerous?
Having too much glucose in the blood clogs up our small blood vessels. Some of the smallest blood vessels in our bodies are the nerves in our fingertips and toes, the filtration system in our kidneys, and the retinas in our eyes. This is why diabetes negatively affects our circulation, limbs, organs, and vision.
In severe cases, uncontrolled diabetes can even lead to amputated limbs, heart or kidney damage, and blindness. Elevated sugar levels also affect our ability to heal. As a result, people with diabetes often take longer to heal from cuts, scratches, incisions, and other wounds.
Diabetes Symptoms
Early symptoms of diabetes are not always easy to pinpoint as being tied to your blood sugar, so it is a good idea to familiar yourself with common diabetes symptoms.
Talk to your doctor if you experience the following diabetes symptoms:
- Frequent urination
- Fatigue
- Persistent hunger or thirst*
- Unexplained weight loss
- Slow-healing cuts
- Pain or numbness in the legs and feet
- Erectile dysfunction**
* People with severe, uncontrolled diabetes often suffer from what feels like an unquenchable thirst. Too much sugar in the blood can mimic dehydration, so our body promotes feeling extremely thirsty to try to rehydrate.
** A common but little talked about consequence of poorly controlled diabetes; when the blood vessels to sexual organs are impacted by elevated glucose, they become clogged and do not allow blood to flow to the area, causing sexual dysfunction.
Testing for Diabetes
It is a good idea to have your blood sugar checked as a baseline. Your doctor will recommend screening frequency based on your age, health, and family history. Testing helps medical providers more accurately gauge your average blood sugar level. It can be done through a finger-prick test or a traditional blood test (i.e., blood taken from a vein). Many insurances cover a glucose test as preventive wellness care at no cost.
Anyone experiencing diabetes-related symptoms should talk to their healthcare provider about getting tested for diabetes. The sooner you have an accurate diagnosis and blood sugar reading, the faster you and your healthcare provider can manage it to get you feeling better.
People who are not currently experiencing noticeable symptoms but are over the age of 40 with additional risk factors for developing diabetes are also encouraged to have their blood-sugar checked. Your weight, chronic conditions, and personal health history factor into your likelihood of developing diabetes and will guide your healthcare provider's recommendations for how often you should test.
Treating Diabetes
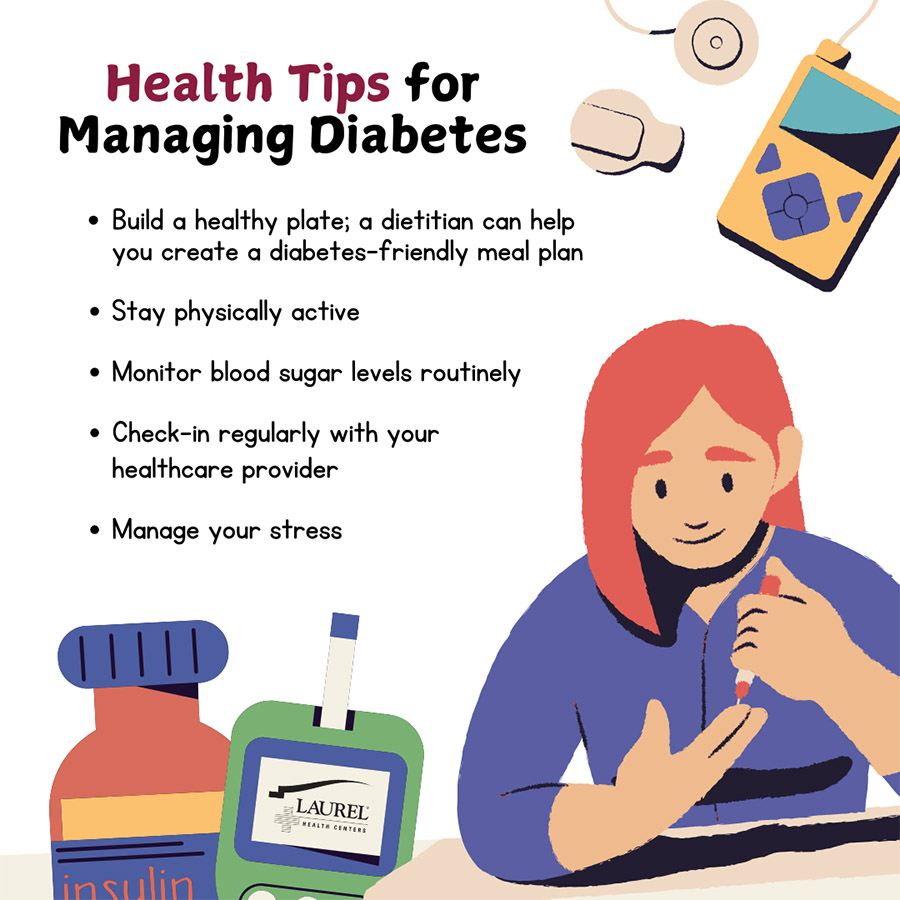
If your test reveals you are at risk for developing diabetes or have untreated or uncontrolled diabetes, don't panic. You and your healthcare provider will develop a plan to better manage your condition. Together, you'll find what works best for you. There are small, simple steps you can take immediately to improve your health and management of diabetes.
One of key components of treating diabetes is examining what we eat and drink. Your doctor may recommend cutting back or cutting out certain drinks or food while you work to get your blood sugar under control.

Soft drinks like soda, juice, or milk can be very high in glucose. Try to focus on drinking enough water instead. How much water we need varies from person to person, but a good starting goal for most adults is 70 ounces of water per day.
Your healthcare provider can give you a personalized hydration recommendation.
Your Laurel healthcare provider can work with you to create a customized plan that fits your unique needs. Your plan to better manage diabetes may include:
- Some changes to your diet or exercise to help you use up and reduce excess glucose
- Support from a diabetes educator or dietitian
- Medication to help control your blood sugar
- Resources to help you stay on track of your health
- Regular monitoring of your blood sugar levels
Should that sound daunting, know that your Laurel healthcare team has your back. The most important thing is to not let fear of a diagnosis or treatment stop you from talking to your doctor or getting tested. The sooner you act, the sooner you can take control of your condition to live a healthier, happier life.
If you are currently experiencing diabetic symptoms, have uncontrolled diabetes, would like to be tested, or want to discuss available medications, make an appointment with the Laurel Health Centers today at 1-833-LAURELHC (1-833-528-7354) or visit our contact page and select the office of your choice.
You may also request a referral to discuss with our registered dietitian Elena Swain, RD, LDN, who is experienced in helping patients manage diabetes and other chronic conditions, at 570-297-3746. She is currently seeing patients at our Mansfield, Towanda, and Troy Laurel Health Centers.
All Laurel Health locations offer both in-person and telemedicine appointments to ensure you can be seen quickly and safely. Laurel Health accepts Medicare, Medicaid, and most major commercial insurances. If cost is a barrier to your care, please talk to our front office staff about our sliding fee program and free insurance enrollment assistance.
For more diabetes health and wellness tips, visit Laurel Health's diabetes education page.